What is a Caudal Epidural Steroid Injection?
Caudal epidural steroid injection is a procedure that is performed to reduce pain due to spinal nerve root irritation or damage.
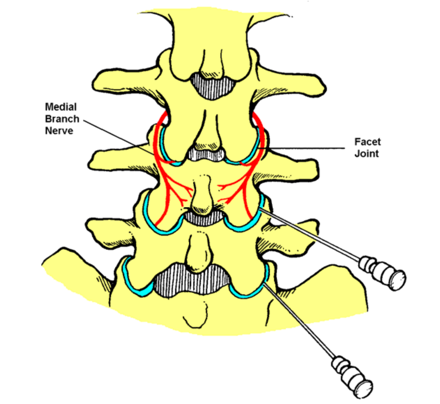
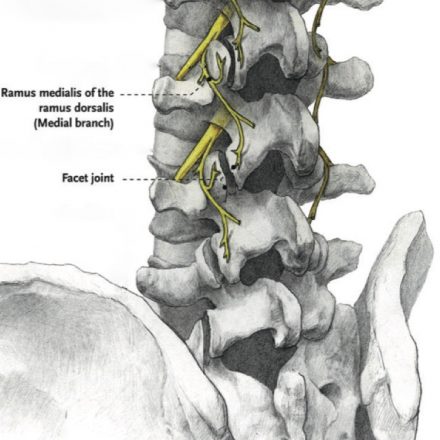
The nerve roots are where the spinal nerves branch off the spinal cord to supply the entire body below the jaw. This neuropathic or nerve pain is often felt in the lower limbs despite the problem being in the bony spinal canal. The cause of the irritation or damage is usually trauma or degeneration of the spine, although there are other causes.
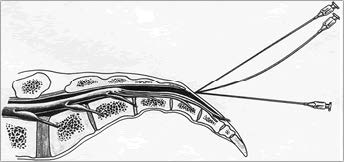
The epidural space surrounds the thick outer covering of the spinal cord (the dura) and extends from the skull to the tailbone. It may be accessed in many ways but the safest route is via an opening in the bones of the tailbone. Some people do not have this opening and may require a higher approach (lumbar epidural steroid injection).
Whichever route is taken, the medications injected are similar. A long-acting steroid medication is injected to reduce pain by decreasing production of inflammatory chemicals and may take a few days to take full effect. The steroid is often mixed with dilute local anaesthetic which acts to distribute the steroid but also washes out the existing inflammatory chemicals and temporarily numbs the nerves to give initial pain relief.
How is the procedure performed?
The procedure is performed in an operating theatre as a day-only stay.
Performing the procedure itself requires about half an hour but you will need to arrive about an hour before the procedure to be prepared for theatre.
A specialist anaesthetist will care for you throughout your procedure. Your anaesthetist will place an intravenous cannula (“drip”) in your hand or arm and administer sedation and oxygen appropriate to the procedure whilst monitoring your vital signs.
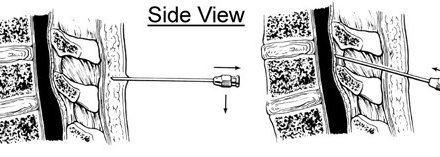
You will be asked to lie face down. Padding will support your head, arms, chest and legs. The procedure will be performed using a sterile technique which involves use of antiseptic solution on your skin, sterile drapes, gown and gloves. The skin will be numbed with local anaesthetic before the needle is inserted. X-rays will be used to place the needle correctly and epidural access will be confirmed by the injection of X-ray contrast before the medication is injected.
What is the likely outcome?
Epidural steroid injection may reduce pain for many months.
This period of reduced pain is often useful to facilitate other therapies (such as active physical therapy or increasing an exercise programme) or to reduce use of harmful medication. The pain may return but the procedure can be repeated, often with similar results.
(Diagram acknowledgement: Walker RS. Painclinic.org)
What are the potential complications?
The procedure is very safe but there are always risks of adverse effects.
Common, short-lived adverse effects include:
- mild pain and bruising at the site of the needle insertion.
- temporary numbness, weakness and bladder disturbance from the local anaesthetic.
Uncommon adverse effects include:
- bleeding (more common if taking blood thinners) or infection.
- severe headache due to puncture of the dura (usually self-limiting but treatable).
- transient steroid-induced flushing, agitation and blood sugar rise (diabetic patients).
Rare adverse effects include:
- nerve damage with lasting effects such as numbness, pain or weakness.
- severe reactions to medications.
- complications related to sedation (please discuss this with your anaesthetist).
The manufacturers did not design the steroid medications specifically for this procedure. However, these medications have been widely used over many years for this procedure without significant complications. Their use is supported by substantial clinical research.
How do I prepare for the procedure?
At the time of booking your procedure it is important that you declare if you:
- are taking any blood thinners, including over-the-counter medications.
- are taking medication for diabetes, especially insulin.
- have an implanted device such as a pacemaker or stimulator.
- could be pregnant (x-rays and medications may cause harm).
A few days before your procedure it is important that you:
- organise an adult to accompany you from hospital and stay overnight with you.
- notify your anaesthetist if you are unwell.
On the day of your procedure it is important that you:
- have nothing to eat for at least 6 hours before your admission time.
- may drink small amounts of water up until 2 hours before your admission.
- take your usual medications unless otherwise instructed.
- have a shower on the morning of the procedure.
What happens after the procedure?
You will recover from your sedation under specialised nursing care. Local anaesthetic from the procedure should minimise post-procedural pain. When it is safe, you will be discharged into the care of an adult. For the next 24 hours you should not drive or operate machinery, care for young children alone or conduct important business.
If you have any unexpected symptoms or side effects following the procedure you should contact your Brisbane Pain Medicine specialist, your family doctor or your nearest emergency department immediately.