What are facet joint injections and medial branch blocks?
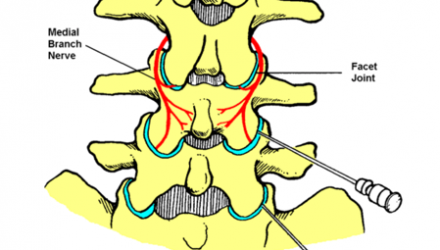
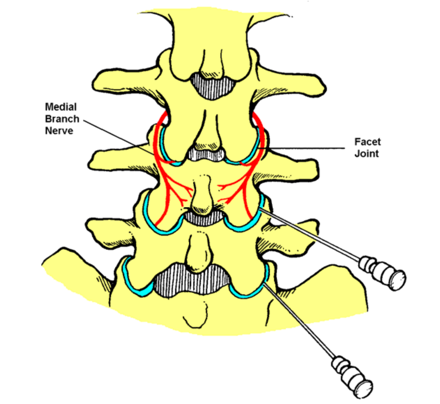
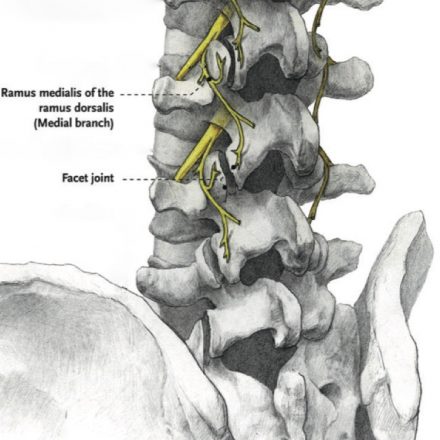
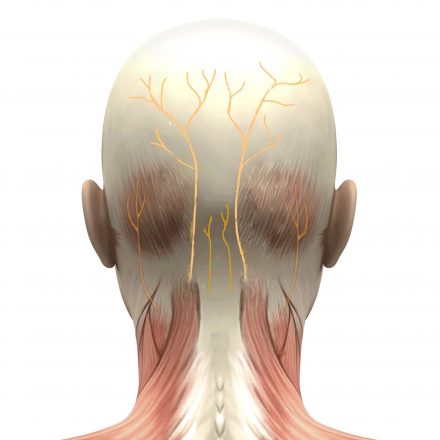
Facet joint injections or medial branch blocks are procedures that are performed to temporarily reduce transmission of pain through very small nerve branches that supply the spinal facet (or zygapophysial) joints.
These joints are bilateral and may be subject to painful osteoarthritis, particularly in the neck and low back where they are weight-bearing joints. Degeneration of these joints is a common cause of low back and neck pain.
During facet joint injections local anaesthetic with or without an injectable steroid are injected into the joints themselves, whereas medial branch blocks involve injection of the same medications around the small nerve branches that supply the facet joints. Both can be helpful for identifying your cause of spinal pain.
How are the procedures performed?
The procedure is performed in an operating theatre as a day-only stay.
Performing the procedure itself requires about half an hour but you will need to arrive about an hour before the procedure to be prepared for theatre.
A specialist anaesthetist will care for you throughout your procedure. Your anaesthetist will place an intravenous cannula (“drip”) in your hand or arm and administer sedation and oxygen appropriate to the procedure whilst monitoring your vital signs.
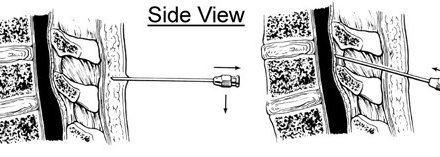
You will be asked to lie face down. Padding will support your head, arms, chest and legs. The procedure will be performed using a sterile technique which involves use of antiseptic solution on your skin, sterile drapes and gloves. X-rays will be used to place the very thin needle correctly before the medication is injected.
What is the likely outcome?
These procedures are usually performed as diagnostic or prognostic injections.
This means that their effects are not expected to last very long but will help your pain specialist determine the underlying cause of your spinal pain and predict your response to therapeutic procedures such as radiofrequency neurotomies. It is therefore important for you to take note of changes (if any) in your pain for especially the first few days after the procedures to report to your pain specialist.
(Diagram acknowledgement: Faculty of Pain Medicine, ANZCA)
What are the potential complications?
The procedure is very safe but there are always risks of adverse effects.
Common, short-lived adverse effects include:
- mild pain and bruising at the site of the needle insertion.
- temporary numbness from the local anaesthetic.
Uncommon adverse effects include:
- bleeding (more common if taking blood thinners) or infection.
- transient steroid-induced flushing, agitation and blood sugar rise (diabetic patients).
Rare adverse effects include:
- nerve damage with lasting effects such as numbness, pain or weakness.
- severe reactions to medications.
- complications related to sedation (please discuss this with your anaesthetist).
The manufacturers did not design the steroid medications specifically for this procedure. However, these medications have been widely used over many years for this procedure without significant complications. Their use is supported by substantial clinical research.
How do I prepare for the procedure?
At the time of booking your procedure it is important that you declare if you:
- are taking any blood thinners, including over-the-counter medications.
- are taking medication for diabetes, especially insulin.
- have an implanted device such as a pacemaker or stimulator.
- could be pregnant (x-rays and medications may cause harm).
A few days before your procedure it is important that you:
- organise an adult to accompany you from hospital and stay overnight with you.
- notify your anaesthetist if you are unwell.
On the day of your procedure it is important that you:
- have nothing to eat for at least 6 hours before your admission time.
- may drink small amounts of water up until 2 hours before your admission.
- take your usual medications unless otherwise instructed.
- have a shower on the morning of the procedure.
What happens after the procedure?
You will recover from your sedation under specialised nursing care. Local anaesthetic from the procedure should minimise post-procedural pain. When it is safe, you will be discharged into the care of an adult. For the next 24 hours you should not drive or operate machinery, care for young children alone or conduct important business.
If you have any unexpected symptoms or side effects following the procedure you should contact your Brisbane Pain Medicine specialist, your family doctor or your nearest emergency department immediately.